We were not prepared for this. Not prepared to cry. Not prepared for an account as moving and revealing as this testimony by Stacey Phelps, a nurse from Alabama who volunteered to work in New York City to fight Covid-19.
Earlier this month, when we asked you to send in your photos and stories “because time was long overdue for the tireless work nurses do to be recognized, acknowledged and appreciated,” we knew we would hear sad and poignant as well as uplifting stories. But no-one spoke to us with such heartbreaking honesty, in such detail, with a voice that resonates so deeply, as Stacey did in her letter.
Stacey is the second winner of our ongoing photo contest, of course — and you can still take part and win $100. But this post is about so much more. Her story conveys the sorrows and struggles of caring for Covid-19 patients in inexcusably dire conditions in sensitive and personal terms, and we are honored to share it with you. People should hear it. So before we say any more, we will let her speak.

“This is truly how it is working as a nurse on the front lines in Brooklyn, New York.”
Stacey Phelps
“It’s been a humbling experience to be a front line worker dealing with this pandemic during its peak. I’m fortunate for good health and the opportunity I had to grow as a nurse, friend, and person while helping those in need.
I came to New York so naive. I came to help these patients with Covid along with all these warrior nurses. I was going to make a difference. I was going to save lives. But that’s not the case here.
It’s crazy here. It’s especially rough here at this Brooklyn hospital I’m working at.. I have questioned myself a lot. Why am I here? What’s my purpose here? What do I need to do?
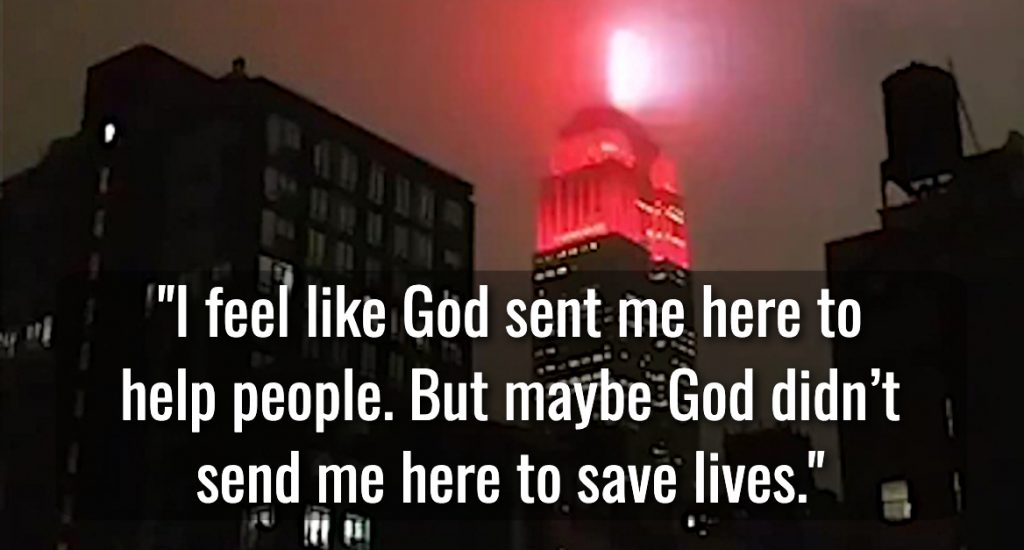
I feel like God sent me here to help people. But maybe God didn’t send me here to save lives. Maybe he sent me here to advocate for patients, to help keep them comfortable and free of pain, to love on them, to help families say goodbye, to give these other nurses time off to rest. I don’t know. I walk in faith, and pray everyday.
My days here in Brooklyn are almost over but Covid isn’t. I keep telling myself to hang on, it’s almost over — but I know it’s not.
“There was no orientation. I was given a badge and a bag of PPE gear and sent to work. I received one face shield for my entire stay … They basically turned every floor into an ICU. They ran out of room in the morgue, so there are refrigerated body trucks outside.”
When I first got here I felt like I walked into a third world country. I have cried more in these past several weeks than I ever have in my entire nursing career. Sure I’ve lost patients before, but not like this. This is truly more than what I thought it would be when I left Alabama the first part of April.
The hospital I’m working at was mandating nurses for 24-hour shifts, with 4 hours off in between, for the past few weeks. Ratios were crazy. When I first got here I had twelve Covid-positive patients with over half of them not stable. Some were even in the hallway.
There was no orientation. I was given a badge and a bag of PPE gear and sent to work. I received one face shield for my entire stay. I was told to keep up with my face shield because they didn’t have extras. I receive one bag of PPE every day with a plastic jumpsuit, N95 mask, gown, booties and scrub cap that I put on at 7am and WEAR for my ENTIRE 12 hour shift. I’ve also been advised to keep my jumpsuit and N95 between shifts in case PPE runs out again and I need to reuse it.
They basically turned every floor into an ICU. They ran out of room in the morgue, so there are refrigerated body trucks outside. Thank God not as many as when I first got here. There are no negative pressure rooms left, so there are units that are just one big room with beds lined up next to each other. There are patients in the hallway lined up against the wall and they have put up privacy curtains.

“Maybe he sent me here to advocate for patients, to help keep them comfortable and free of pain, to love on them, to help families say goodbye… I don’t know. I walk in faith, and pray everyday.”
There is no Pyxis, so all the meds come from pharmacy in plastic bags with patient sticker labels on them. Drips do not come pre-made, we figure out how to mix the drips before we hang them. There are very few IV pumps so you have to do the old school drop method and count them just right. With my OCD I end up counting far more than most.
There are no ETT secures, so tubes are secured by wrapping them with surgical tape and then wrapping the tape around the patient’s head. If a patient needs a central line, the resident has to call the doctor to put it in, so it is not uncommon to have very sick patients on critical care drips running through 22 or 24 gauge IVs which may be in their foot or leg. And I’ve gotten good at putting them in too.
Patients are being coded everyday and if a patient codes while on a vent, we leave them on the vent instead of bagging them to reduce exposure risk. There is a code team that is supposed to come to every code, but there are sometimes multiple codes going on at the same time, so it can take awhile for them to arrive.
I’ve noticed one thing about these patients, and that is they seem stable or even appear to be getting better, and then suddenly code without warning.
When you get an off day all you want to do is sleep, but dreams keep waking you. You try to hide the mental detritus this virus has left on your mind.
You sweat all day and hardly get a chance to stay hydrated. You hold your urge to pee in fear of taking your PPE off. I truly think I have hypercapnia from keeping my N95 on for 12 hours. I’ve been trying to take at least two breaks and go outside for air. But sometimes that’s hard to do.
When you get an off day all you want to do is sleep, but dreams keep waking you. You try to hide the mental detritus this virus has left on your mind.
This is truly how it is working as a nurse on the front lines in Brooklyn, New York.”

This is not over. Nurses are still fighting. Patients still surviving. Families still grieving.
“My days here in Brooklyn are almost over but Covid isn’t,” Stacey wrote us on May 15. “I keep telling myself to hang on, it’s almost over — but I know it’s not.”
And it really isn’t. The news headlines have moved on, as the country faces a new heartrending crisis — but over a thousand Covid-19 patients died yesterday. Another thousand died the day before. Over 20 thousand new cases were recorded yesterday. Families are grieving the deaths of 100,000 people.
Some countries have announced a time of mourning for the tens of thousands who died; here we tend to want to move on. But nurses are still fighting on the front lines. Helping people survive … and comforting those who will not.
They are surviving the onslaught of the experience themselves, too, sometimes barely. “When you get a day off, all you want to do is sleep,” Stacey writes, “but dreams keep waking you.” We will not echo platitudes about self-care here. But we will plead with anyone who reads this to be kind… to your colleagues, to your nurse friends, and most of all: to yourself.
