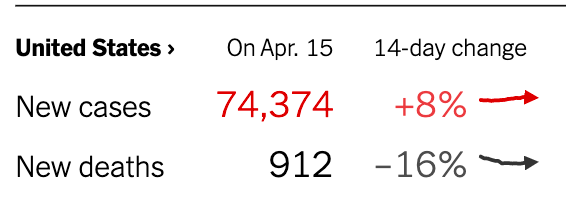
It’s a powerful symbol. Every day now, for weeks already, if you scroll down the New York Times homepage, you see the same thing. It’s a very plain graphic, with just three lines of text, underneath the header “Tracking the Coronavirus”.
In red: “New cases”. Up. Every day, the number is up.
In black: “New deaths”. And every day, it’s down. By a lot. Usually a double digit percentage.
That’s the power of the vaccination campaign against COVID-19. At this point, 39% of Americans have received at least one dose. Not enough to stop the pandemic in its tracks. But enough to give many of the most vulnerable people at least some protection. And that’s translating into fewer people dying. Into lives saved, day after day.
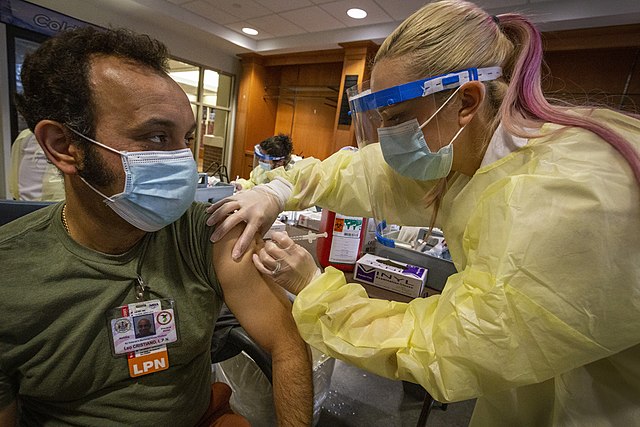
All the nurses who have already been part of this immense effort can be proud of their work. President Biden promised 100 million vaccinations in his first 100 days in office. Thanks to the tireless work of healthcare workers, that goal was reached on day 58, and now the objective is 200 million.
For that to work, healthcare workers around the country will have to redouble their efforts. More nurses still will be needed on the frontline.
You can find COVID-19 vaccination jobs right here on NurseRecruiter.com. In this post we will give you some useful employer shortcuts to help you find the right one for you, quickly. But we also want to inform you about what to expect, what is at stake, and where we can expect challenges to mount. Only interested in the jobs? Jump straight to the employer shortcuts.
Race against the clock
131 million Americans have received at least one dose so far; 84 million are fully vaccinated. Mind-bending numbers. Records were shattered on April 10, when 4.6 million people were vaccinated in a single day.
But we have a long way to go. In New Hampshire, more than half of the population has received at least one dose. But it’s only just over a quarter in Mississippi.
No less now than before, it also remains a race against time. Many of the most elderly and at-risk populations now enjoy significant protection, but hospitals are seeing ever more people in their 30s and 40s admitted with severe cases of COVID-19.
“This is how we turn the tide of this pandemic – one shot at a time.”
Nellie Darling, medical student at Georgetown UNIVERSITY
By now, the highly contagious B.1.1.7 or ‘British’ variant has become dominant in the U.S. Other, even more problematic strains that were first reported in Brazil and South-Africa are looming, and it’s still not entirely certain how effective each of the currently used vaccines are against them. The longer the virus circulates among the population, the greater the risk that further and harder to contain variants will emerge.
The job will get harder
Overall vaccine hesitancy is declining. The number of people taking a wait-and-see attitude has halved since December. But the smaller shares of people saying they definitely won’t get the vaccine, or only if required, stubbornly keep adding up to some 20%.
That could prove crucial, because more than 15-20% of the population holding out “could mean the difference between the U.S. achieving herd immunity and resuming normal life or variants of COVID-19 getting second and third winds, leading to new lockdowns or restrictions on life”.
Even before you get to those people, however, the job already gets harder once we get to the point where most of the people who couldn’t wait to get the vaccine — and had the skills and resources to find one — have been covered.
“How to vaccinate everyone not eagerly lined up for a shot” is “a dizzying public health challenge,” the New York Times warned, which “encompasses persuading skeptics, calling people who do not realize they are now eligible, and making vaccines accessible for homebound patients, overstretched working families and people in rural areas and minority communities”.
COVID-19 vaccination: from volunteers to travel nurses
That’s why people from across the health care sector have joined the effort. School nurses have provided their time and expertise when vaccination sites were established in schools. National Nurses United is deploying volunteers in a COVID-19 Vaccine Stand By Team to underfunded community clinics in places like South LA. Medical students at institutions like PCOM South Georgia are volunteering their time. Georgetown University medical and nursing students, faculty and staff vaccinated more than 1,000 people in one weekend.
But there are Covid vaccination travel nursing opportunities as well! By mid-March, for example, the California Department of Public Health was already deploying almost 2,000 travel nurses to help with vaccinations.
In San Bernardino County alone, there were 160 SnapNurse workers by the end of the month. “We had a sense of relief when we saw their five buses arrive,” the county’s public health program manager told the LA Times. “It’s just what we needed. We wouldn’t have been able to do it without them.”
That’s not necessarily just going to be a temporary phenomenon either. Some of the pharmacy chains and medical clinics which have gone on hiring sprees “appear to be treating these thousands of newly created jobs as permanent positions,” NBC News reported. The spectre of COVID-19 evolving sadly might mean this is not “just a temporary, ‘mission to the moon’ type situation where you have this huge mobilization and then it’s over,” labor economist Julia Pollak told them — “some of these programs may be longer lasting than many of us think”.
Employer shortcuts: find vaccination travel nursing jobs!
Here on NurseRecruiter.com, four companies regularly post COVID-19 vaccinator job openings. So before we move on to discuss what challenges the vaccination campaign needs to address next, check out their employer profiles to see which of their current vaccination job opportunities appeals to you! Or go straight to our vaccine jobs page to see all current openings, from any employer and agency, in one place.
 |
Constellis regularly posts job openings for RNs and LPNs to administer COVID-19 vaccines. Locations range from Vermont to Alabama. Depending on the position and the location, salaries can be up to $60/hour plus travel and hotel costs. “This is one of the most important humanitarian missions of our time” |
|
|
Whether you’d like to work in Miami or Minneapolis or even up in Anchorage, SPD Staffing is calling for nurses to deploy as COVID-19 vaccinators ASAP. On top of the hourly rates they’re currently offering a health & welfare fringe benefits stipend as well as a travel/housing stipend for those venturing further from home. |
 |
|
 |
Citing an “immense need,” Colorado-based healthcare staffing firm Comcentric has been posting a range of COVID-19 vaccination positions for local RNs and LPNs in cities across the state. Unlike some of the other openings which involve long hours, many of these are Mon-Fri day shifts of 8 hours, 3-5 shifts a week. |
|
|
Having grown exponentially as a business, Accessible Home Health Care is now recruiting RNs and LPNs to take up positions across Florida as COVID-19 Vaccine Nurses. In addition to an hourly rate of $35-50, travelers are eligible for travel and hotel cost reimbursement. |
 |
|
Nurses have a special role to play
When it comes to the COVID-19 vaccines, doctors and nurses are in a special position to encourage, empower and educate. According to Kaiser Family Foundation (KFF) survey data, eight in ten Americans say that, in the end, it’s their doctors they’ll turn to when deciding on the COVID-19 vaccine — and we know that nurses consistently rank as one of America’s most trusted professions.
That’s why the KFF’s Drew Altman argued that “one of the most important messages vaccine reluctant Americans can hear” right now is: “Your doctor and your nurse trusts the COVID-19 vaccine; you can too.”
The trick here, a Journal of Advanced Nursing (JAN) article about “the nursing contribution to COVID‐19 mass vaccination programmes” argues, is to move the conversation away from emotive controversy, where people end up feeling “pressured or stigmatized rather than having their concerns addressed”. Because that doesn’t help anyone!
Instead, the focus should be on establishing a trusting relationship, facilitating open and personalized discussions, exploring and responding to concerns, and “signposting to credible sources of information [about] the safety, efficacy and purpose of the vaccine”.
Which sounds great, but what does an actual day administering COVID-19 vaccines look like? “If you’ve ever participated in a flu clinic, you already have a good idea of the general procedures,” explains Christine Contillo, a public health nurse in Bergen County, NJ — “but COVID-19 vaccination clinics involve some additional challenges”.
The two-dose requirement for most vaccines means more patient education and follow-up, for example. You don’t let patients leave until they’ve been observed for reactions. Add the limited time window for the administering of some vaccines after thawing and of course the need for social distancing, and it’s all a little different.
Roberta Heale, an NP who “jumped at the chance” to take part in COVID-19 vaccine immunization clinics, has recounted the experience on the BMJ Evidence-Based Nursing blog, describing the two different models she’s seen. The common denominator, however, is an “an air of enthusiasm and determination” among the workers as well as all those coming in for their shot, who are “almost universally.. thrilled to be receiving their COVID vaccines”.
There are also training tools to help. The CDC provides several “clunky but useful” COVID-19 Vaccine Training Modules which explain the use of the Janssen, Moderna and Pfizer vaccines. In Texas, partners from Lone Star College, Texas Christian University, Texas Tech University, and Baylor Scott & White Health have developed a “Just-In-Time COVID-19 Vaccination Training Module”.

Harder to reach — divides by race and politics
A couple of handy training modules, however, are not going to solve the broader challenges ahead. The ways that were used so far to quickly get as many doses as possible rolled out are not going to work everywhere in the next stages. “You can’t build a vaccination program on chain pharmacies and hospitals and then expect it to work in low-income or rural communities,” explained vaccine expert Peter Hotez, pointing out that those areas often don’t have many of either.
Overall, vaccination data so far show significant differences between communities. When 32% of white Americans had already received at least one vaccine dose, just 19-20% of Black and Hispanic Americans had. That’s all the more concerning because those communities have been more at risk of COVID-19. In California, for example, over half of Covid cases and almost half of Covid deaths have been Latino residents.
The story is in part about lack of access. “People from hard hit communities often have limited access to digital tools needed to schedule an appointment,” the DiversityNursing blog explained, “and often information about vaccine registration is only available in English.” But it’s also partly about greater vaccine hesitancy, born in part of a troubled history of the treatment of black people in medicine and health care which created a legacy of distrust.
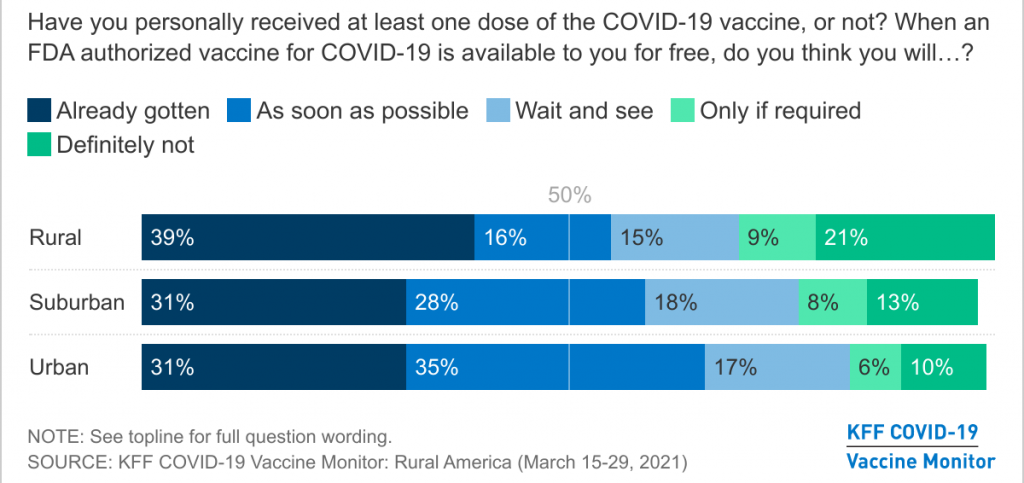
Vaccine hesitancy is a major challenge elsewhere as well. “Republican men, rural residents and adults under 45” are among those “more likely to refuse”.
In fact, the differences in vaccination rates across the country have “mainly broken down along political lines,” with both interest in the vaccine and actual vaccination rates lower in counties which voted for Trump. The KFF COVID-19 Vaccine Monitor found that some three in ten Republicans and White Evangelicals in rural America say they will “definitely not” receive a COVID-19 vaccine.
It even got to the point where health workers and officials in rural Iowa and Wyoming had to cancel volunteers or vaccine deliveries because there was too little interest. That’s why top officials and experts are making a point of appearing on outlets like Fox News and Newsmax and reaching out to faith leaders — without judgment. “You listen to the audience, you understand where they are and you address their concerns,” former CDC director Tom Frieden explained.
“Nobody will be safe until everybody’s vaccinated”
Beyond those broad demographic strokes, there are particularly challenging groups which have been underserved or are hardest to reach.
Mass vaccination sites and online appointment systems are great for “those who have the benefit of flexible schedules… reliable transportation and internet access”. But for the most impoverished who don’t have a car or gas money, especially in rural areas without much in the way of public transport, popping by a vaccination site is a little more daunting. They might not even realize the vaccination is free.
Digital literacy is an issue too. The reliance on the Internet for people to register for a vaccination or schedule an appointment has made the process a lot more efficient, but it also throws up more hurdles. Hurdles that no number of “vaccine angels” or “vaccine hunters” volunteering their time to help others find spots can realistically solve.
Despite federal government assurances that everyone, no matter their immigration status, is eligible for the vaccine, many undocumented immigrants have run up against more restrictive rules and procedures which individual states may establish to verify people’s eligibility.
“Most of our agricultural workers, day laborers and domestic workers have not had access to the vaccine,” the executive director of a South Dade immigrant workers’ center in Florida told the Miami Herald.
There are other groups, too. COVID-19 has torn through prison populations with particular ferocity. But “fewer than 20% of state and federal prisoners have been vaccinated” and “in some states, prisoners and advocates have resorted to lawsuits to get access”.
Some cities have started vaccinating thousands of homeless people in shelters. In Washington, DC, some of those homeless people now even serve as “peer educators”, encouraging others and dispelling the conspiracy theories that are rampant in this population. But efforts to vaccinate those who live in the streets are still very rare. Public health experts like Dr. Patrick Kachur are left hoping that the Johnson & Johnson vaccine, which only requires one dose, will be a game changer for this group.
All of this is a long-term problem. Dallas County Judge Clay Jenkins pointed out that vaccinating the homeless “makes all of us safer,” and that really holds much more broadly. The dean of Brown University’s School of Public Health, Ashish Jha, put it more bluntly: “nobody will be safe until everybody’s vaccinated”.
Whatever it takes
The Biden administration last month dedicated “another $10 billion to try to drive up vaccination rates in low-income, minority and rural enclaves throughout the country”. But in the end, this is not about what politicians in DC decide, but about what local communities on the ground do. And they have been creative!
Check out these examples:
— New York City added a mobile vaccine bus to the twenty mobile vans they had already deployed, to bring “hundreds of doses a day literally to your doorstep”. Together with the city of New York, ROAR New York is operating a vaccine bus to vaccinate restaurant workers and restaurant delivery workers across the city.
— The Osage Nation in Oklahoma bought two 30-foot “medical R.V.s” to drive up to every small town. “We tried to remove every obstacle to people who were sitting on the fence,” said Dr. Ronald Shaw, in what the New York Times described as “a house-by-house campaign against misinformation and wariness, waged with long conversations and patience“.
— In Philadelphia, the nurse-led Family Practice and Counseling Network (FPCN) started using leftover “angel” doses for home visits to vaccinate vulnerable homebound patients.
— Not far away, Kevin Emmons of Rutgers University-Camden School of Nursing and his team started hosting pop-up vaccine clinics in housing complexes, going “door-to-door asking if there’s anyone who is elderly, homebound, or without internet access who would like to get the vaccine”.
— On the other side of the country, the Umoja Health ‘pop up’ vaccination site in Oakland goes for a community-based approach which, UCSF associate professor of epidemiology Dr. Kim Rhoads explained, proved its worth with COVID-19 testing. The organization is known within the local Black community — “street-certified,” as volunteer A.J. Burleson called it. The pop-ups are accessible and fun. Its volunteers are familiar neighborhood faces. And they’d first done on-the-ground outreach to let people know and sign them up.
Have you heard about innovative or inventive vaccination initiatives, that will help bring vaccines against COVID-19 to all people and places that haven’t been covered much yet? Let us know in the comments!